The global health community is in a period of fierce research and innovation to address the world’s most pressing environmental issues. Those of us in respiratory health are particularly invested – our wellbeing is undeniably linked to the air we breathe and the health of our planet.[1]
The climate crisis, pollution and other environmental factors contribute to the burden of chronic respiratory diseases like asthma and chronic obstructive pulmonary disease (COPD).[2] At the same time, caring for millions of people with these conditions carries an environmental impact, as is the case for nearly all healthcare services.[3] We need to pursue two important goals in parallel: protecting our environment alongside protecting healthcare for people with respiratory diseases. This has increasingly become a key consideration for policymakers introducing important environmental legislation in Europe.
For instance, the decision of EU co-legislators to phase out fluorinated greenhouse gases (F-Gas) by 2050 and a proposed ban on per- and polyfluoroalkyl substances (PFAS) through the REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals) Regulation aim to achieve significant progress towards the EU’s green agenda, climate action and future global health.[4],[5] Yet discussions amongst policymakers and stakeholders have shown we must be mindful of any unintended impact upon the health of individuals,[6] including potential unintended consequences of such legislations, especially when it comes to inhaled medicines.
Many inhaled respiratory medicines fall within the scope of such proposed legislations, in particular due to the propellants they use to facilitate delivery of the medicine to a patient’s lungs.[6] We need to work across sectors to protect the health of patients who rely on these essential medicines. As we have seen with the F-Gas Regulation, this includes legislation and timelines that allow for completion of regulatory reviews, and support the availability of and safe transition to more environmentally friendly versions of current standard of care medicines using next-generation propellants with near-zero global warming potential.

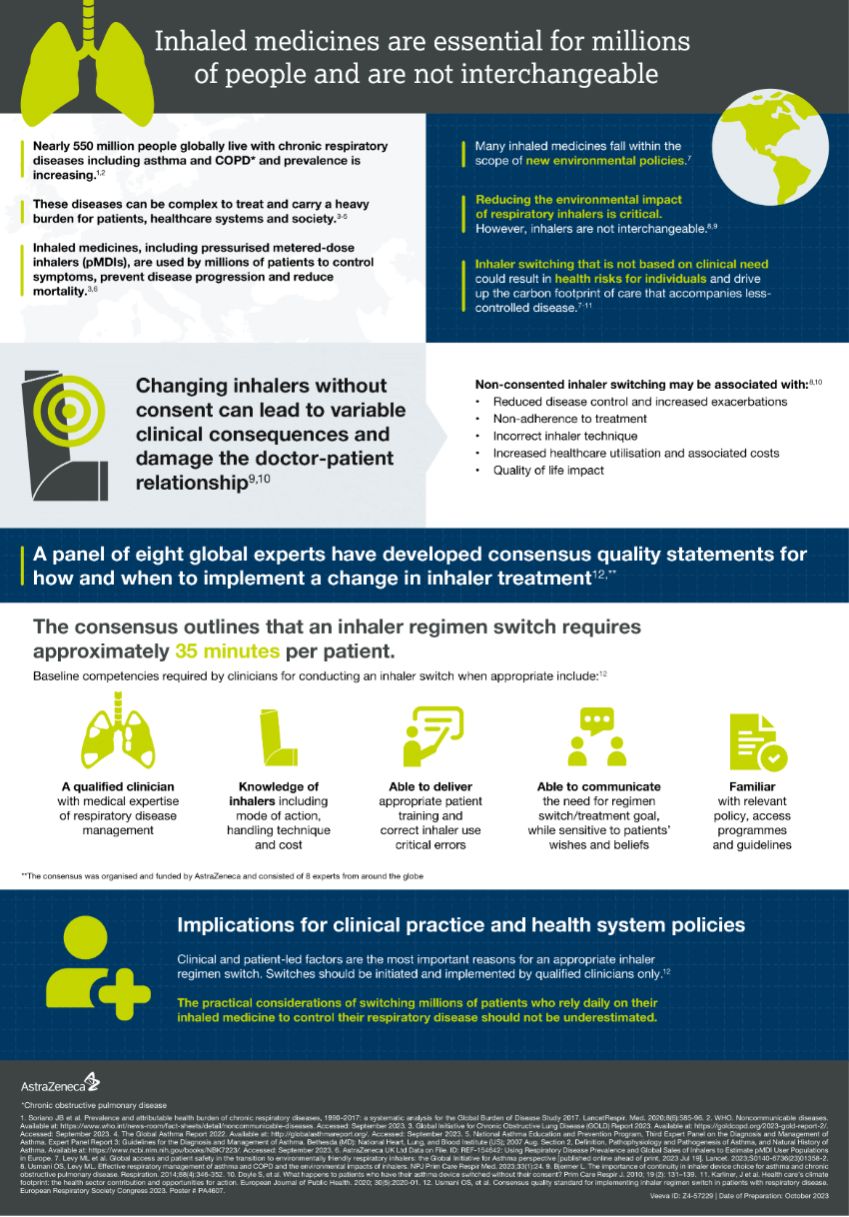
While the environmental impact of specific treatments merits consideration, it is important to note that simply switching respiratory patients to alternative medicines is not a viable option. A variety of inhalers are currently available, and each has its specificities. There is no universal and ideal inhaler that would suit all patients: each has their own specific abilities, skills and preferences that need to be considered on an individual basis to personalise the choice of the inhaler and provide the appropriate education on how it should be used.[6],[7],[8] In fact, abrupt switching could result in health risks for individuals and drive up the carbon footprint of care that accompanies less-controlled disease.[6],[8],[9],[10]
 Click to see the full infographic
Click to see the full infographic
A new consensus* presented by respiratory experts at the European Respiratory Society International Conference states that if an inhaler switch is to happen, it should only be done by a trained healthcare provider following consultation with their patient on symptom and disease control, capabilities for device use and preferred choice of regimen.[10] When a patient is able and willing to use several device types properly, and when quality care can be maintained, the choice should of course go to the most environmentally friendly.
Rather than systematically switching all patients to a given type of inhaler, we should be looking to one of the most effective tools already available today to drive down the environmental burden of respiratory care: implementing evidence-based treatment guidelines and quality standards to support the best individualised care possible for people with diseases like asthma and COPD. The better managed patient’s diseases are, the better their health and quality of life, and the less emergency and other hospital services are needed, therefore driving down the environmental impact.[6],[8]
When it comes to prioritising patient outcomes and advancing a greener agenda – both are achievable in respiratory care. The greenest situation is when a patient knows how to use their inhaler medicine properly and their disease is well controlled.

Nicolas Roche is a Professor of Respiratory Medicine at Paris Cité University and Head of the Department of Respiratory Medicine, Cochin Hospital, APHP Centre, Paris, France.
*The consensus was organised and funded by AstraZeneca and consisted of 8 experts from around the globe.
Authors have not received payment for involvement in this article. Over the past years, Nicolas Roche or his institute have received payments and/or research funds and fees from companies including AstraZeneca.
[3] J Karliner et al. Health care’s climate footprint: the health sector contribution and opportunities for action. European Journal of Public Health. 2020; 30(5):2020-01.
[6] Levy ML, Bateman ED, Allan K, et al. Global access and patient safety in the transition to environmentally friendly respiratory inhalers: the Global Initiative for Asthma perspective [published online ahead of print, 2023 Jul 19]. Lancet. 2023;S0140-6736(23)01358-2.
[7] Usmani OS. Choosing the right inhaler for your asthma or COPD patient. Ther Clin Risk Manag. 2019;15:461-472.
[8] Usmani OS, Levy ML. Effective respiratory management of asthma and COPD and the environmental impacts of inhalers. NPJ Prim Care Respir Med. 2023;33(1):24.
[9] Bjermer L. The importance of continuity in inhaler device choice for asthma and chronic obstructive pulmonary disease. Respiration. 2014;88(4):346-352.
[10] Usmani et al. Consensus quality standard for implementing inhaler regimen switch in patients with respiratory disease. European Respiratory Society Congress 2023. Poster # PA4607.
Organised and funded by AstraZeneca
Sign up to The Parliament's weekly newsletter
Every Friday our editorial team goes behind the headlines to offer insight and analysis on the key stories driving the EU agenda. Subscribe for free here.